By Tahmid Hasan
In Bangladesh, NCDs are estimated to account for 67% of all deaths. In low and middle-income countries, urbanization has been identified as one of the crucial underlying reasons for the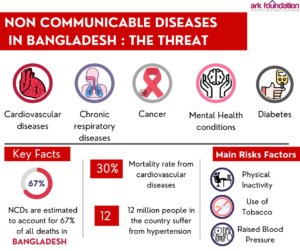 increasing trends of NCDs. Bangladesh has also been experiencing rapid urbanization for the past two decades. The urban population of Bangladesh has increased exponentially, from 21.3 million in 1990 to 53.1 million in 2014, and it is expected to reach 112.4 million by 2050. Almost one-third of the urban population lives in densely populated slums with poor housing conditions. The socioeconomic and living conditions in these urban slums are very substandard, and in most cases, the residents do not have access to the basic amenities required for urban life. It puts them at the risk of contracting different types of communicable and non-communicable diseases. The need to focus on NCDs in the urban health care system increases when the growth of the urban population has been so rapid.
increasing trends of NCDs. Bangladesh has also been experiencing rapid urbanization for the past two decades. The urban population of Bangladesh has increased exponentially, from 21.3 million in 1990 to 53.1 million in 2014, and it is expected to reach 112.4 million by 2050. Almost one-third of the urban population lives in densely populated slums with poor housing conditions. The socioeconomic and living conditions in these urban slums are very substandard, and in most cases, the residents do not have access to the basic amenities required for urban life. It puts them at the risk of contracting different types of communicable and non-communicable diseases. The need to focus on NCDs in the urban health care system increases when the growth of the urban population has been so rapid.
The majority of deaths from NCDs in Bangladesh can be attributed to cardiovascular diseases, diabetes, cancers, and chronic respiratory diseases. Cardiovascular diseases account for the highest mortality rate among NCD patients in Bangladesh. Besides, most NCDs have associated risk factors that have significant health implications. Risk factors such as inadequate intake of fruits and vegetables, tobacco use, unhealthy diet, physical inactivity, obesity, sodium intake, and high blood pressure have been identified among urban adults in Bangladesh. According to Bangladesh NCD Risk Factor Survey 2018, most of the population has one or two risk factors, and a substantial proportion of the population has three or more risk factors.
 The presence of NCDs among urban slum dwellers worsens their already poor-quality living standards. Due to high costs and significant out-of-pocket health expenditure, urban poor communities have limited access to good quality health care in Bangladesh. As such, the prevalence of NCDs puts many families in financial hardships and exacerbates their economic situation. Although Bangladesh has witnessed success in terms of providing equitable healthcare services for the rural population, healthcare for the urban poor remains highly inaccessible and inequitable. There has also been a lack of care towards Non-Communicable Diseases (NCD), specifically in the urban setting.
The presence of NCDs among urban slum dwellers worsens their already poor-quality living standards. Due to high costs and significant out-of-pocket health expenditure, urban poor communities have limited access to good quality health care in Bangladesh. As such, the prevalence of NCDs puts many families in financial hardships and exacerbates their economic situation. Although Bangladesh has witnessed success in terms of providing equitable healthcare services for the rural population, healthcare for the urban poor remains highly inaccessible and inequitable. There has also been a lack of care towards Non-Communicable Diseases (NCD), specifically in the urban setting.
The rural poor now have better access to health services compared to the poor in urban settings. People in the rural areas can visit the community clinics in villages to get treatment for basic diseases and maternal health. Rural health complexes also now have dedicated NCD corners available, following the WHO recommendation to integrate NCD in to primary healthcare. These NCD corners provide prevention, screening, and treatment for common NCDs at the Upazila/sub-district level in its three-tiered Primary Health Care (PHC). There are still major gaps in the availability and accessibility of NCD services in the primary and secondary levels of the health system due to the scarcity of the government’s health budget.
However, health facilities like community clinics are largely absent for the urban poor. For availing of health care, they have the option to either go for expensive private facilities or neglected public hospitals. The existing provision of urban primary health care falls under the purview of the Ministry of Local Government, Rural Development and Co-operatives (MoLGRD), which aggravates the situation. Health is one of the many priorities of the MoLGRD, and NCD care remains mostly absent in the primary health care centres under their authority.
neglected public hospitals. The existing provision of urban primary health care falls under the purview of the Ministry of Local Government, Rural Development and Co-operatives (MoLGRD), which aggravates the situation. Health is one of the many priorities of the MoLGRD, and NCD care remains mostly absent in the primary health care centres under their authority.
There are many national guidelines and protocols formulated by the government to improve the situation of NCDs, and NCDs appear in key government policy documents. However, in reality, there is a lack when it comes to the implementation of such protocols, especially at the primary care level of the urban health centres. Moreover, there is no mechanism of record-keeping and following up of NCD patients, and no formal referral pathway, causing a lack of standardized care for patients suffering from NCD across urban areas. In addition, there is a lack of digitalization of urban health data.
 The Government certainly prioritizes NCDs and hence, it has adopted the multi-sector action plan for prevention and control of non-communicable diseases. It points out the key strategies and sets priorities for the primary stakeholders. It has been developed following the key strategic plans like the 8th Five-Year Plan, 4th Health, nutrition, and population strategic investment plan (HNPSIP), and other crucial legislation and guidelines. If the strategies pointed out in these documents can be implemented then Bangladesh will move a long way towards improving the NCDs care in urban settings. We must remember that the COVID-19 has had a serious impact on the lives of the urban poor. Most of them have seen a decline in their income levels. Besides economic issues, COVID-19 put the fragile health conditions of the urban poor at further risk. As COVID unfolded, it exposed our longstanding weaknesses in the health sector. However, while it exposed the lacking of health centers in providing basic health care, it has also left some room to utilize this experience and improve the existing situation. With a constantly growing urban population, we must focus on the improvement of the care of NCDs and follow the existing guidelines to mitigate the associated risk factors. The government needs to focus on further research to generate evidence-based decisions to strengthen the urban health systems and ensure healthy environments to facilitate behavioural change.
The Government certainly prioritizes NCDs and hence, it has adopted the multi-sector action plan for prevention and control of non-communicable diseases. It points out the key strategies and sets priorities for the primary stakeholders. It has been developed following the key strategic plans like the 8th Five-Year Plan, 4th Health, nutrition, and population strategic investment plan (HNPSIP), and other crucial legislation and guidelines. If the strategies pointed out in these documents can be implemented then Bangladesh will move a long way towards improving the NCDs care in urban settings. We must remember that the COVID-19 has had a serious impact on the lives of the urban poor. Most of them have seen a decline in their income levels. Besides economic issues, COVID-19 put the fragile health conditions of the urban poor at further risk. As COVID unfolded, it exposed our longstanding weaknesses in the health sector. However, while it exposed the lacking of health centers in providing basic health care, it has also left some room to utilize this experience and improve the existing situation. With a constantly growing urban population, we must focus on the improvement of the care of NCDs and follow the existing guidelines to mitigate the associated risk factors. The government needs to focus on further research to generate evidence-based decisions to strengthen the urban health systems and ensure healthy environments to facilitate behavioural change.