Written by: Asiful Haidar Chowdhury (Senior Research Fellow)
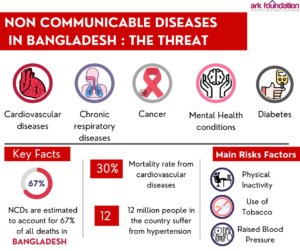
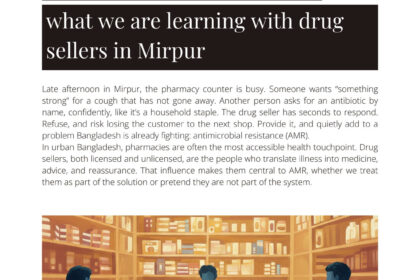
Late afternoon in Mirpur, the pharmacy counter is busy. Someone wants “something strong” for a cough that has not gone away. Another person asks for an antibiotic by name, confidently, like it’s a household staple. The drug seller has seconds to respond. Refuse, and risk losing the customer to the next shop. Provide it, and quietly add to a problem Bangladesh is already fighting: antimicrobial resistance (AMR).
In urban Bangladesh, pharmacies are often the most accessible health touchpoint. Drug sellers, both licensed and unlicensed, are the people who translate illness into medicine, advice, and reassurance. That influence makes them central to AMR, whether we treat them as part of the solution or pretend they are not part of the system.
With support from the CHORUS Innovation Fund (Round 2), ARK Foundation is implementing a study on drug sellers and AMR in urban health settings of Bangladesh, with technical support from the University of Leeds and financial support from the UK Foreign, Commonwealth & Development Office (FCDO). The goal is practical: understand how formal and informal drug sellers dispense antibiotics in the city, what pressures shape those decisions, and what realistic pathways exist to strengthen knowledge and practice in ways that reduce inappropriate antibiotic use.
Starting with the ground reality: mapping 1,100 pharmacies
Before asking drug sellers about antibiotics, we needed to understand the landscape they work in.
ARK researchers were trained and conducted a pharmacy mapping exercise across 15 wards of Mirpur, covering 1,100 pharmacies between 28 March 2024 and 4 April 2024. What emerged was a clear snapshot of a mixed marketplace: 551 pharmacies (50%) were licensed under the Directorate General of Drug Administration (DGDA), while 549 (50%) were operating without a license.
That 50/50 split is not just a statistic. It is a reminder that “the system” is not one neat, fully regulated structure. Antibiotics move through both formal and informal channels, and any serious AMR response in cities must take that reality seriously. If half the pharmacy network sits outside formal licensing, then efforts that focus only on licensed outlets will miss a large part of where antibiotic decisions happen.
The trust question: why a DGDA letter mattered
During mapping, many drug sellers were open to conversation but cautious about participation in later activities. A recurring message was simple: if the regulator supports the work, participation feels safer.
In response, ARK engaged with relevant personnel in DGDA’s AMR cell through several meetings, shared the study objectives and planned activities, and ultimately received a DGDA letter of support to facilitate implementation. On paper, it is a short document. In practice, it helped remove a barrier that was shaping willingness to engage. It also signaled something broader: that addressing antibiotic dispensing practices requires not only evidence, but relationships and institutional alignment.
Listening at scale: a survey with 400 drug sellers
With the mapping list as a sampling frame, a structured survey was conducted between September and October 2024 among 400 drug sellers, randomly selected from the mapped pharmacies. The survey explored drug sellers’ knowledge, attitudes, and day-to-day practices related to antibiotic dispensing, as well as their interest in training.
In a magazine piece, it is tempting to jump straight to results. But this work is not just about “what people know.” It is about the conditions that shape what people do: customer expectations, competition between shops, informal norms, and the risks drug sellers perceive when they say no. Capturing that reality requires both numbers and context.
Seeing the wider system: interviews with key stakeholders
To understand the broader environment drug sellers operate within, ARK conducted four in-depth interviews with potential stakeholders, including representatives from DGDA, CDC, and senior public health leaders with experience in antimicrobial and AMR-related work.
These conversations focused on gaps and opportunities for strengthening drug seller capacity, the practical constraints that influence dispensing behavior, and the economic and contextual incentives that can drive inappropriate antibiotic sales. The point was not to assign blame. It was to understand how policy, enforcement, market dynamics, and public expectations intersect at the pharmacy counter.
Turning experience into story: participatory videos with drug sellers
Data matters. Stories do too, especially when the aim is to shift understanding, build empathy, and open space for change.
As part of the CHORUS Innovation Fund work, ARK organized a five-day participatory video development workshop from 18-22 May 2025 at the DISA Training Center in Mirpur, Dhaka. Drug sellers from nine pharmacies participated in interactive sessions facilitated by ARK researchers and a digital media specialist.
The workshop was designed to surface real pressures and decision points: why antibiotics get requested, why they get dispensed, what rules feel unclear or impractical, and what trade-offs drug sellers feel forced to make. Through guided storytelling and role-play, participants translated lived experience into scripts that reflected the realities of antibiotic dispensing in an urban setting.
From this process, two scripts were drafted. After review and revision with local and international experts, both scripts were finalized. Filming then took place with the participation of drug sellers at their own pharmacy sites in two areas of Mirpur. Following editing, two participatory videos were produced.
Bringing people into the room: showcasing and feedback
The videos were not created to sit on a hard drive. A showcasing event was held with drug sellers, community representatives, and DGDA officials to screen the videos and gather feedback on quality and content. That feedback is being incorporated, and the videos will be finalized after revisions.
Alongside the showcasing, group discussions were conducted with participating drug sellers to document their reflections on the workshop and filming process, including what felt useful, what was challenging, and how they experienced telling their own stories in a structured, public-facing format.
What this is building toward
AMR is often discussed as a technical crisis. At the pharmacy counter, it looks like something else: a negotiation between health needs, customer demands, business survival, and uneven regulation.
This study is assembling multiple forms of evidence, from mapping and surveys to stakeholder perspectives and participatory videos, to support a more realistic response to antibiotic misuse in urban Bangladesh. The intention is two-fold: strengthen drug seller capacity in ways that fit their working realities, and support dialogue with regulators and other stakeholders on what is feasible, fair, and effective.
Over time, the evidence and materials generated through this work are expected to help shape training approaches, sensitization efforts, and collaborative discussions that recognize drug sellers not as outsiders, but as a group with influence, constraints, and potential to contribute to healthier antibiotic use in the city.
Originally published in ThinkSpace Vol:1 (February, 2026)