Have you ever wondered what would happen if no medicine were effective to treat illnesses, caused by bacteria, fungi, viruses, and parasites? I am sure you have never thought about it. But it could happen because of a process known as “Antimicrobial Resistance or AMR”.
We will discuss about AMR later. First, let us familiarize ourselves with a new term that I have come to know a few days ago.
“A Tragedy of the Commons.”
Tragedy of the Commons occurs when the shared, limited resources of a community are exhausted, depleted, and exploited by its people due to their personal gain, even though the depletion of that very resource would eventually bring loss to the community in the longer term. In short, people neglect the greater well-being of the community in order to achieve personal gain. Overfishing without thinking the loss of reproduction of aquaculture would be the classic example of the Tragedy of the Commons.
But how is this term relevant to Antimicrobial Resistance (AMR)?
Antimicrobial Resistance (AMR) occurs when antimicrobials such as antibiotics, antifungals, and antiviral are no longer effective against the disease-causing microbes and bacteria. These microbes have evolved (changed) in order to find ways of surviving antimicrobial treatments. When this happens, we say that the microbes are resistant to antimicrobials. In biology we call these changes mutations. They happen naturally and gradually over time but anything that is stressful to a microbe can force it to change or mutate more quickly. The use of antimicrobials is incredibly stressful for a microbe. Drugs like antibiotics are designed to kill microbes like bacteria and so the microbe will do anything it can to protect itself. The more antimicrobials are used the more microbes will fight back and find ways to survive the medicines – this is AMR.
Antimicrobial Resistance is fast become a new example of the ‘Tragedy of the Commons. This is because many people use antibiotics and other antimicrobials to treat common illnesses, they don’t follow health professional’s advice on dosage, or they use them in the livestock farming to increase the growth and productivity of animals. However, this ‘misuse’ of antibiotics could result in fatal consequences in the future because of AMR. We might soon be faced with an era where antimicrobials are no longer able to treat our illnesses because many microbes have become resistant to them.
As several studies suggest, people often utilize antibiotics and other antimicrobials without following the usage guidelines created by professionals such as the World Health Organization. This means microbes are being exposed to antimicrobials regularly but often not long enough to kill them. This in turn means microbes can find ways to change (mutate) to survive the medicine. This trend of AMR is increasing at a concerning rate worldwide.
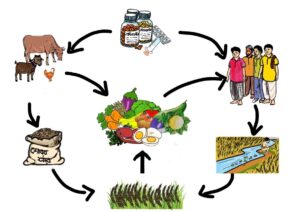
Because microbes can move around in our soil, water and pass between human and animal bodies, resistant microbes can quickly spread from human to human, human to animal, animal to human and across geographic areas. This is therefore the right time to focus on tackling Antimicrobial Resistance from the ‘One Health’ perspective which includes humans, animals and the environments.
Antimicrobial Resistance not only regresses us to a pre-antimicrobial era (Antibiotics /antimicrobials like antimalarials were only commonly used since the 1940s) when people died of infections now treatable with antibiotics, but also will have a devastating effect on the world’s economy.
According to a recent report “Drug-Resistant Infections: A Threat to Our Economic Future (2017)” by the World Bank, Global GDP may be reduced by 3.8 percent if AMR is high, whereas in the optimistic case scenario, the global economic output might shrink by 1 percent by 2030 and 1.1 by 2050. If uncontrolled, the AMR could cause the world GDP to fall lower than the figures we saw in the 2008-2009 financial crisis. This cost is due to an increased spending on health care infrastructure and response to drug resistant infections in human health and food producing animals.
Bangladesh as a country might face both the direct and indirect costs of diseases as a result of Antimicrobial Resistance. Direct costs include the resources used to treat the disease, such as prolonged or multiple hospitalizations and medication costs for multiple courses, or more expensive drugs. Bangladesh has already suffered from the escalated burden of out-of-pocket expenditure for healthcare with nearly no existence of any social safety net or insurance. According to the BNHA (1997-2015), a large share of out-of-pocket health expenditure of people goes on medicines. Many people are forced into impoverishment due to catastrophic health expenditures every year in the country. With the efficacy of antibiotics and other antimicrobials declining, both the medication cost and the extended hospital stays will contribute to the increased cost of healthcare, pushing more people towards impoverishment. Moreover, drug-resistant infections will require more and more advanced diagnostic tests to identify and treat diseases resulting in a further cost burden to the general population.
In the case of indirect cost, people will suffer from higher morbidity in the longer term which would lessen the overall production of the country.
Unregulated, misuse and overuse of antibiotics and other antimicrobials in livestock production, animal health and agricultural processes will have similar consequences. Animal disease will be harder to treat, require more veterinary attention and potentially more expensive courses of medication. If drug resistant infections in food producing animals are fatal, we could also face a decreased supply of livestock and thus increased prices of major sources of protein such as meat, milk and eggs.
There are other costs associated with AMR as well. We still do not know about these costs with certainty. There is a risk that those costs could be far higher than the current best estimates by the economists. Assume that there is a 1% increase in resistance to a certain drug, then it would be very important for us to know what pathogen is exhibiting that resistance, what type of infection the pathogen causes, the current and future health burden of that infection, how transmissible the resistance gene and infection are, and whether alternative treatments are available and how costly they are. Because the cost of increased resistance and the threat it poses is uncertain. Thus, it is complex to measure the actual economic impact of AMR.
This grim situation posed by AMR calls for immediate global action. Over-the-counter dispensing and selling of antibiotics remain a major problem in Bangladesh. This action contributes to making the AMR situation worse because people can access antimicrobials without health professional’s advice on usage. The Directorate General of Drug Administration has already suggested a couple of actions to contain the problem. Additionally, strengthening the monitoring framework and proper implementation of the law from the supply side (Provider aspect) coupled with strong community awareness among general people (Consumer aspect) could help to tackle this overlooked pandemic.
It is not too late to invest in tackling AMR to protect the future generation from untreatable infections. Otherwise, interventions that we are using for a long time and get comfortable with such as major surgery, management of injuries and efficient food production might get much more expensive and challenging for us.
Author- Md Badruddin Saify, Research Assistant, ARK Foundation